Introduction to conservative mastectomies
The definition of conservative mastectomies was first introduced in the medical literature by Dr. Nava et al., of the Istituto Nazionale dei Tumori Milano, Italy (1).
Nowadays, the aesthetic result for primary treatment of breast cancer patients is as important as oncological safety and must be the actual goal of the breast surgeon. In this context, new surgical procedures emerged as “conservative mastectomies”, expanding the concept of a better outcome for breast conservation procedures.
In the last 50 years, breast surgery evolved from maximum tolerable treatment with aggressive and mutilating interventions, like radical mastectomy, to minimum effective treatment, and from an anatomical concept of cancer spread to a biological concept.
Conservative mastectomies incorporate the advantage of tumor and total gland excision, as in a traditional total mastectomy, with improvement in the esthetic result through conservation of the skin envelope and the nipple areolar complex (NAC). The use of anatomical expanders and high cohesive silicone implants ensures high quality immediate reconstruction in these patients, but autologous tissue can also be used to fill the empty skin pocket after gland resection.
At first glance, conservative mastectomy (CM) may appear similar to subcutaneous mastectomy, which was first described by Freeman (2), and it’s still used for risk reduction.
However, there are two significant differences: the thickness of the skin flaps and the presence of retroareolar tissue.
As a curative procedure, CM incorporates the entire breast parenchyma, sparing only the skin, or in selected cases utilizing NAC preservation (3).
NAC ischemia and necrosis are some of the expected complications; however, solutions for these are technically simple. The issues relevant to the technique are oncological safety and long-term follow-up.
Three different techniques for CM that have been oncologically validated are:
- —skin-sparing mastectomy (SSM) (4);
- —nipple-sparing mastectomy (NSM) (5);
- —skin-reducing mastectomy (SRM) (6).
CM by using any of these three techniques is indicated when mastectomy is unavoidable, or when the patient prefers a mastectomy instead of breast conservation surgery (BCS). CM is also indicated for small breasts, when more than 30% of the breast volume must be resected and the cosmetic result after radiotherapy (RT) will be poor.
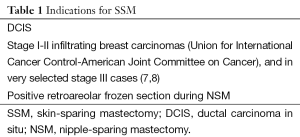
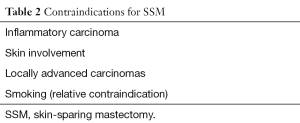
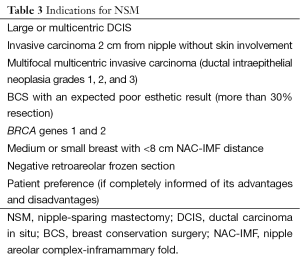
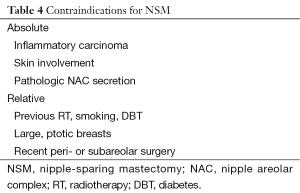
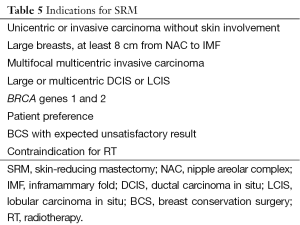
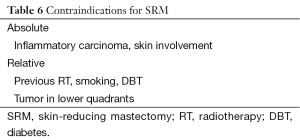
Preserving skin, NAC, and the inframammary fold (IMF) enables improved immediate reconstruction with both implants and autologous tissue (Tables 1-6).
Full table
Full table
Full table
Full table
Full table
Full table
The difference in terminology between these approaches to breast cancer is important.
BCS with Previous RT has been accepted since the 1980s as a standard therapeutic modality for low-grade breast cancer.
This is a partial breast resection that includes lumpectomy (removal of the lump), quadrantectomy (removal of one quarter, or quadrant, of the breast), and segmental mastectomy (removal of the cancer, some of the breast tissue around the tumor, and the lining over the chest muscles beneath the tumor). A universally accepted basic oncological priority is to maximize disease control and obtain a satisfactory cosmetic outcome.
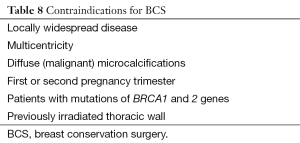
Different oncoplastic planning approaches and techniques can be used to improve the final cosmetic result in BCS (9,10), with rigorous selection of candidates. In addition to a complete history and physical examination, the most important guideline includes preoperative diagnostic imaging, including magnetic resonance imaging (MRI) (Tables 7,8).

Full table
Full table
Desirable cosmetic result in BCS and in CM is mandatory and a key factor in selecting an approach, when oncologic safety is guaranteed with either modality (11).
Different CM techniques appear to combine oncological safety with high quality cosmetic outcomes (12,13), and this procedures are an extending concept of breast preservation. Cooperation between breast and reconstructive surgical teams is still necessary, and both teams must be aware of the oncological and plastic surgery approaches and oncoplastic technique for each case (14). CM offers today an important psychological benefit and oncological safety for a large group of breast cancer patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Nava MB, Catanuto G, Pennati A, et al. Conservative mastectomies. Aesthetic Plast Surg 2009;33:681-6. [PubMed]
- Freeman BS. Technique of subcutaneous mastectomy with replacement; immediate and delayed. Br J Plast Surg 1969;22:161-6. [PubMed]
- Spear SL, Willey SC, Feldman ED, et al. Nipple-sparing mastectomy for prophylactic and therapeutic indications. Plast Reconstr Surg 2011;128:1005-14. [PubMed]
- Singletary SE, Kroll SS. Skin-sparing mastectomy with immediate breast reconstruction. Adv Surg 1996;30:39-52. [PubMed]
- Verheyden CN. Nipple-sparing total mastectomy of large breasts: the role of tissue expansion. Plast Reconstr Surg 1998;101:1494-500; discussion 1501-2. [PubMed]
- Nava MB, Cortinovis U, Ottolenghi J, et al. Skin-reducing mastectomy. Plast Reconstr Surg 2006;118:603-10; discussion 611-3. [PubMed]
- Chang EI, Ly DP, Wey PD. Comparison of aesthetic breast reconstruction after skin-sparing or conventional mastectomy in patients receiving preoperative radiation therapy. Ann Plast Surg 2007;59:78-81. [PubMed]
- Cao D, Tsangaris TN, Kouprina N, et al. The superficial margin of the skin-sparing mastectomy for breast carcinoma: factors predicting involvement and efficacy of additional margin sampling. Ann Surg Oncol 2008;15:1330-40. [PubMed]
- Carlson GW. Skin sparing mastectomy: anatomic and technical considerations. Am Surg 1996;62:151-5. [PubMed]
- Carlson GW, Bostwick J 3rd, Styblo TM, et al. Skin-sparing mastectomy. Oncologic and reconstructive considerations. Ann Surg 1997;225:570-5; discussion 575-8. [PubMed]
- Veronesi U, Stafyla V, Petit JY, et al. Conservative mastectomy: extending the idea of breast conservation. Lancet Oncol 2012;13:e311-7. [PubMed]
- Rancati A, Gonzalez E, Angrigiani C, et al. Oncoplastic options in breast conservative surgery. Gland Surg 2013;2:163-9. [PubMed]
- Rancati A, Gonzalez E, Dorr J, et al. Oncoplastic surgery in the treatment of breast cancer. Ecancermedicalscience 2013;7:293. [PubMed]
- Toth BA, Lappert P. Modified skin incisions for mastectomy: the need for plastic surgical input in preoperative planning. Plast Reconstr Surg 1991;87:1048-53. [PubMed]


