Using intraoperative laser angiography to safeguard nipple perfusion in nipple-sparing mastectomies
The superior cosmetic results of nipple-sparing mastectomies (NSM) account for the steady increase in use of these operations. Cancer recurrences involving the nipple-areolar complex (NAC) have been reassuringly low. Wang et al. reviewed 981 cases of total skin-sparing mastectomy (TSSM) and immediate breast reconstruction, reporting an overall 5-year locoregional recurrence of 3% and no recurrences in the NAC (1). Similarly, others have reported equally low rates of NAC recurrences, less than 1%, thus counterbalancing some of the high rates of occult involvement of the nipple with tumor as discussed below (2-5). The oncologic safety of this procedure is further demonstrated in BRCA-positive patients who are at higher risk for developing breast cancer and in patients after neoadjuvant chemotherapy (6).
Preservation of the NAC gives way to the possibility of recurrence therein and especially of a Paget’s type of recurrence. Boneti and coauthors reported comparable local recurrence rates among 227 patients undergoing SSM and 281 NSM, 6% and 5% (P=0.89), respectively (7). Lohsiriwat et al. reported 7 (0.8%) of 36 local recurrences were Paget’s disease among 861 NSM with electron beam intraoperative radiotherapy (8). The average time interval to Paget’s recurrence was 32 months (range, 12-49 months). Risk factors for this type of recurrence included invasive ductal carcinoma with extensive in situ component, negative hormonal receptor status, high grade, and HER2-positive subtype.
Contraindications to nipple-sparing mastectomy are straightforward, namely Paget’s disease, nipple retraction or direct involvement by tumor (9). However, in the absence of clinical changes, occult involvement of the NAC remains a concern. Tumor extension to the NAC has ranged widely, from as low as 6% to 38%, if only studies with 100 or more patients are considered (2,10-13). Clinically occult nipple involvement has been related to retroareolar location or distance of index lesion, size of primary tumor, lymph node metastases, lymphovascular invasion and HER-2 overexpression (4,14). Brachtel et al. found that invasive ductal histology with DCIS had the highest association with nipple involvement, while age, multifocality, BRCA positive status and neoadjuvant chemotherapy did not (2). Moreover, this group found that that the absence of carcinoma in retroareolar sampled tissue correlated with the absence of carcinoma in the nipple, a sensitivity of 0.8 and a negative predictive value of 0.96. Recently, Eisenberg et al. reported their experience regarding occult nipple involvement in 325 NSM performed at Weill-Cornell Medical Center (15). Biopsies taken from the base of the nipple were free of tumor in 117 prophylactic mastectomies while 14% of 208 therapeutic mastectomies showed tumor cells, including five cases of LCIS. Central location of tumor and four or more positive nodes were the only two factors associated with nipple margin status. The intraoperative positive frozen section rate was considerably lower, 4.8%, a practical point to consider, as these assessments are preliminary and may require nipple resection once permanent sections are finalized. Interestingly, another 12 cases underwent nipple resection based on other considerations (cosmetic, close margin or technical reasons), finding malignant cells in an additional two cases.
Evaluation of skin perfusion
Skin flap ischemia is the most common postoperative complication affecting all skin sparing mastectomies (7). The rates for skin-sparing and NSM are 6.2% vs. 7.1%, respectively. The work by Chirappapha and colleagues underscore the risk of skin and NAC necrosis occurring in patients with larger breasts (16). They suggest a protocol of slow expansion with tissue expanders or the use of autologous musculocutaneous flap to prevent ischemic complications.
Visual inspection and bleeding along skin flap edges have been the traditional methods used to judge adequate skin perfusion in the operating room. Surgeons typically excise discolored, cyanotic-appearing skin or trim skin to a bleeding edge. Visual inspection can be deceptive leading to underestimation or overestimation of ischemia. A case in point is shown in Figure 1, where it is likely that the presence of vascularized autologous tissue beneath the area of ischemia lessened the severity of evolving skin necrosis. Reversible conditions such as vasospasm, cooling, or low circulating volume, may affect the appearance of skin flaps. Consequently, many plastic surgeons avoid being overly aggressive in resecting areas with seemingly marginal perfusion. Beyond visual inspection, Doppler devices, tissue oxymetry, and fluorescein have been used to evaluate perfusion but have not been shown to be completely reliable in clinical practice (17). Fluorescein dye angiography has more significant side effects, 15-minute delay to visualization, and longer half-life (18). Moreover, although less expensive, it has the added disadvantage of not providing quantitative information and single use per operation.

Objective evaluation of skin perfusion is critical to the recognition of tissues with poor blood flow. Intraoperative angiography can provide real-time information on tissue perfusion, complementing visual assessments and clinical decisions (17,19). Indocyanine green (IC-GREEN™, ICG) (Pulsion Medical Systems SE, Germany; 2.5 gm/mL) is a fluorescent dye approved in the US for injectable use with reported rare allergic side effects have (20). The SPY Elite™ imaging system (Novadaq Technologies, Inc., Ontario, Canada) utilizes an infrared camera to capture the inflow of blood, which is visualized within seconds after intravenous administration on computer screen. The early iterations of this system monitored flow continuously for only a 60-second segment, while the upgraded equipment extends imaging over 270 seconds. This technology is being used in many centers to assess breast, mastectomy skin or myocutaneous flap perfusion in order to guide skin resection, resulting in a decrease of ischemic complications (21). Phillips et al. prospectively compared the fluorescein angiography to an older version of ICG-based angiography (18). The sensitivity of the two methods was similar but SPY imaging was superior in terms of specificity, as well as positive and negative predictive values. In their study, fluorescein was more likely to overestimate areas of skin flap necrosis than SPY imaging.
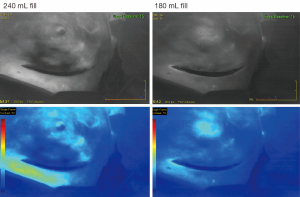
Evaluation of skin perfusion during mastectomy operations continues to be received with some skepticism. The sequence of events shown in Figure 2, illustrate the utility of SPY imaging as an intraoperative tool in a case of immediate post-mastectomy reconstruction. Compromised perfusion involving part of the areola and inferior mastectomy flap can be identified on the photograph associated with 240 mL volume in the tissue expander. Removal of 60 mL, restored adequate blood flow to those areas. Accordingly no ischemic complications were noted clinically during the postoperative course. More recently, Duggal and colleagues demonstrated that ICG angiography significantly lowered reoperation rates (14.1% vs. 5.9%) and skin necrosis (23.4% vs. 13.0%) in their experience on 184 skin-sparing but non-nipple sparing, mastectomies (19). Moreover, they demonstrated a cost-benefit advantage to the use of this technology when considering overall hospitalization and reoperation charges.
Nipple-areola ischemia
Dissection of involved or at-risk breast tissue along the subdermal plane is standard practice in mastectomy operations. The primary goal in NSM is removal of all the breast tissue in the same manner without compromising the oncologic safety of the more aesthetic operation. Technically, NSM are more challenging and the larger skin envelopes more prone to ischemic complications. Impaired perfusion leads to discoloration, and partial or complete nipple necrosis (Figures 1,3). Thin skin flaps and pressure exerted by prosthetic reconstruction, can add to the compromise of skin blood flow in the post-operative period (1). Groups that knowingly leave breast tissue below the base of the nipple add intraoperative radiotherapy target the NAC (22). Alternatively and more commonly in the United States, the practice of coring out nipple ducts for NSM has been adopted in order to address concerns about the potential hazards of leaving breast tissue at risk in association with the NAC.
Rusby et al. studied the cross-sectional anatomy of the nipple to investigate the distribution of terminal ducts coursing through (23). By leaving a 2 mm rim of nipple skin, they calculated that 96% of the total number of ducts would be excised, while a 3 mm peripheral rim would only excise 87% of ducts. In addition, they demonstrated the viability of the nipple by staining vascular endothelium and assessing blood vessels. About 50% of the nipple vessels on cross-section were preserved with as little as a 2 mm rim of nipple skin. Their observations provide useful anatomic information indicating that excision of the duct bundle should not compromise the arteriolar blood supply of nipple dermis.
The incidence of ischemic complications involving the NAC vary from study to study. Less than complete NAC necrosis affected 37.5% of women in this series with 14 of 15 of these cases healing simply with local wound care and only one requiring nipple reconstruction (24). While tissue loss is a major complication of nipple-areolar ischemia, reversible ischemia or transient ischemia that results in epidermolysis and epidermal sloughing can result in permanent discoloration of the nipple and areola (Figure 3).

Partial and full nipple necrosis was reported by Mallon et al. as 6.3% and 2.9%, respectively (4). A study from University of California San Francisco presented a lower overall rate of partial nipple necrosis, 2.0%, with only ten cases (1.5%) out of the total 657 NSM complicated by complete NAC necrosis and loss. Limiting the extent of periareolar incisions to 30% of the areolar circumference and, using a superior areolar and inframammary incisions were helpful changes in their intraoperative technique for the remaining 557 cases. This was reflected in a reduction in rates of nipple necrosis from 13% to 1.8% (P<0.0001) when comparing earlier with later cohorts of patients (25,26). In a recent update, the same group reported full nipple necrosis in 1% and superficial necrosis or epidermolysis in 3.5% (1). Minimizing pressure on skin flaps via the use of tissue expanders and optimizing coverage of prosthetics with acellular dermal matrix or muscle led to improvements in outcomes.
Incisions and nipple perfusion
The location of incision for NSM is influenced by the breast volume and ptosis, the distance between the NAC and inframammary fold, the presence of prior scars and the type of reconstruction. However, patient and physician preference and desire to maximally camouflage the incisions also play a role. From a technical standpoint, in order to resect all the breast tissue extending from the clavicle and beyond the anterior axillary line, an infra-mammary fold incision must be made sufficiently wide to allow access. As such, many surgeons favor the radial-lateral or inferior vertical-radial incisions, including partial but limited extension around the areola. Recently, in a pooled analysis Endara et al. described, NAC necrosis of 8.8% for radial and 9.1% for inframammary incisions compared to 17.8% for periareolar and 81.8% for transareolar incisions (27). Based on these results the inframammary fold or the radial approaches were recommended.
Garwood and colleagues were able to reduce NAC complications by limiting the extent of periareolar incisions to less than one-third of the circumference of the areola or by avoiding the NAC entirely (28). In this study, two cohorts of two sequential time periods were analyzed. Nipple survival rates rose from 80% to 95% (P=0.003) and necrotic complications decreased from 30% to 13% (P=0.01). Here too, incisions involving >30% of the NAC were an independent risk factor for skin necrosis. They noted that improved NAC viability with limited periareolar incisions is consistent with not disrupting the subdermal vascular plexus that supplies the nipple. Most of their subsequent cases since their early experience have been performed through inframammary or limited superior areolar incisions, with a subsequent reduction of NAC complications to 1.8% in their 2012 series (26).
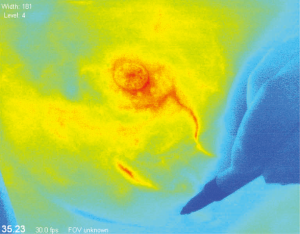
Our group at Stanford uses SPY Elite™ imaging intraoperatively to perform baseline assessments of the skin circulatory anatomy, with the aim of avoiding injury to critical skin vessels before making an incision in nipple or skin-sparing mastectomies. Moreover, we have incorporated this technology in other challenging situations where a breast lumpectomy for cancer is combined with a reduction mammoplasty procedure. Figure 4 shows a pre-incision sequence depicting arterial inflow to the NAC at the 5 o’clock position. Perfusion to the NAC would have been significantly compromised if an inferior-based periareolar incision were used. Instead, the real time obtained images altered the surgical approach and guided the surgeon to employ an inframammary incision.
Nipple perfusion patterns
We have been using SPY Elite™ imaging as an adjunct to breast cancer operations combined with reconstructive surgery. One of the ways this technology is helpful, is by informing surgeons in real-time, the circulatory anatomy of the NAC. Intraoperative post-mastectomy imaging revealed absent perfusion in the area of the NAC (Figure 5). The arterial ingress pattern demonstrated filling from the underlying breast tissue without any seeming contribution from surrounding cutaneous blood vessels. These observations led to a more extensive examination of NAC perfusion.
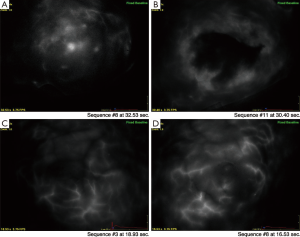
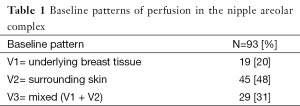
Three patterns of arterial-arteriolar filling were defined qualitatively: V1, underlying breast tissue; V2, surrounding skin; and V3, dual or V1 and V2 (29). Among the 39 cases initially reported, 7 of 39 (18%) breasts demonstrated a V1 perfusion pattern in the NAC, 18 (46%) a V2 pattern and 14 (36%) a V3 pattern. The proportion of cases in each category at baseline remained similar in a larger cohort with 93 breasts as shown in Table 1. Specifically, the majority or 48%, demonstrate a V2 pattern while 20% have V1. In our original series of 39 breasts, 71% with a V1 pattern underwent NAC removal based on intraoperative ischemic changes vs. 11% for the V2 group. The differences in rates of NAC loss by perfusion classification were significant (P=0.0003). We now report an additional 15 breasts undergoing a one-stage NSM (Table 2). In this combined analysis, 56% of breasts with a V1 pattern had intraoperative nipple resection compared to 3.4% with V2 patterns. Postoperative loss of the NAC has been lowered to 2%, excluding those removed intraoperatively. With a larger sample size, interactions with other factors such as type of incision may further our understanding and our ability to predict ischemic complications. In summary, preservation of adequate NAC perfusion in NSMs is likely dependent on a confluence of factors ranging from breast volume, ptosis, location and type of incision as well as circulatory anatomy. The latter is evaluable and unique in every individual.
Full table

Full table
Staged devascularization of the NAC
Ischemic complications and skin loss detract from the cosmetic goals of NSM. Women with larger or ptotic breasts seeking NSM, experience more ischemic complications (14,30). Devascularization or vascular delay has been used in surgery for many years as a means of improving blood flow through tissues via hypertrophy of existing vessels or the formation of new collaterals (31). Jensen et al. have ingeniously applied a two-stage approach for women at higher risk of developing ischemia based on ptosis, previous scars, and active cigarette smoking (32). The first stage entails undermining the NAC with some surrounding skin along the mastectomy plane. A subnipple biopsy is also included at this time to confirm the absence of tumor involving the NAC. Seven to 21 days later, the mastectomy is completed. During this timeframe, it is presumed that the surgical wound enhances blood flow. In their study of 20 patients, none of the 28 tumor free NAC that were devascularized were lost and only two patients experienced superficial ischemia or epidermolysis after the delay procedure. A variation on this technique was published by Palmieri and colleagues (33). They advocate the use of tumescence and endoscopic cauterization along the subareolar plane during a first operative procedure.
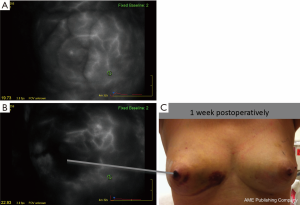
We have adopted a similar approach and are studying the changes in patterns of perfusion that occur in the course of this two-stage vascular delay approach. Using intraoperative ICG-based SPY Elite™ imaging, recovery of deficits in skin perfusion can be observed. Slow filling areas recover over 3 to 4 weeks either due to hypertrophy and vasodilatation of existing dermal blood vessels or neovascularization. Figure 6 illustrates a woman with a BMI of 33 who underwent a two-stage NSM. The baseline images demonstrated areas of hypoperfusion affecting the NAC and correlate with zones of epidermolysis on the 1-week post-devascularization clinical examination, that healed completely over the following weeks. This approach will surely facilitate the use of NSM for more patients and minimize ischemic complications and reoperations.
Reconstruction and NSM
Immediate reconstruction has certainly gained favored over the last two decades, with a preference in many centers toward a two-stage procedure whereby a tissue expander is placed at the time of ablative surgery, with the advantage of gauging the pressure exerted on the skin flap. Plastic surgeons face greater challenges when performing NSM. The larger skin envelopes predispose patients to more ischemic complications. Acellular dermal products are used to enlarge the limited cover provided by the pectoralis major muscle, forcing parts of the NAC and skin flaps to be in direct contact with non-perfused tissue. Clearly, the greater demand for NSMs challenges the surgical community to conduct this type of operation for patients previously considered poor candidates. The adoption of periareolar pexy in women with moderately ptotic breasts is an added example of how these technical problems can be resolved (30).
Conclusions
Technological advances have made it possible to evaluate tissue perfusion in real time. This is extremely useful in the case of NSM where preservation of blood flow is most critical. The challenge before us is to extend the benefits of natural appearing NSM to women with prior breast surgery, large and ptotic breasts.
Acknowledgements
None.
Footnote
Conflicts of Interest: Irene L. Wapnir, Shannon Meyer, Geoffrey C. Gurtner have consulted for Novadaq Inc. The other authors have no conflicts of interest to declare.
References
- Wang F, Peled AW, Garwood E, et al. Total skin-sparing mastectomy and immediate breast reconstruction: an evolution of technique and assessment of outcomes. Ann Surg Oncol 2014;21:3223-30. [PubMed]
- Brachtel EF, Rusby JE, Michaelson JS, et al. Occult nipple involvement in breast cancer: clinicopathologic findings in 316 consecutive mastectomy specimens. J Clin Oncol 2009;27:4948-54. [PubMed]
- Petit JY, Veronesi U, Orecchia R, et al. Risk factors associated with recurrence after nipple-sparing mastectomy for invasive and intraepithelial neoplasia. Ann Oncol 2012;23:2053-8. [PubMed]
- Mallon P, Feron JG, Couturaud B, et al. The role of nipple-sparing mastectomy in breast cancer: a comprehensive review of the literature. Plast Reconstr Surg 2013;131:969-84. [PubMed]
- Poruk KE, Ying J, Chidester JR, et al. Breast cancer recurrence after nipple-sparing mastectomy: one institution's experience. Am J Surg 2015;209:212-7. [PubMed]
- Peled AW, Irwin CS, Hwang ES, et al. Total skin-sparing mastectomy in BRCA mutation carriers. Ann Surg Oncol 2014;21:37-41. [PubMed]
- Boneti C, Yuen J, Santiago C, et al. Oncologic safety of nipple skin-sparing or total skin-sparing mastectomies with immediate reconstruction. J Am Coll Surg 2011;212:686-93; discussion 693-5. [PubMed]
- Lohsiriwat V, Martella S, Rietjens M, et al. Paget's disease as a local recurrence after nipple-sparing mastectomy: clinical presentation, treatment, outcome, and risk factor analysis. Ann Surg Oncol 2012;19:1850-5. [PubMed]
- Lohsiriwat V, Petit J. Nipple Sparing Mastectomy: from prophylactic to therapeutic standard. Gland Surg 2012;1:75-9. [PubMed]
- Morimoto T, Komaki K, Inui K, et al. Involvement of nipple and areola in early breast cancer. Cancer 1985;55:2459-63. [PubMed]
- Lüttges J, Kalbfleisch H, Prinz P. Nipple involvement and multicentricity in breast cancer. A study on whole organ sections. J Cancer Res Clin Oncol 1987;113:481-7. [PubMed]
- Santini D, Taffurelli M, Gelli MC, et al. Neoplastic involvement of nipple-areolar complex in invasive breast cancer. Am J Surg 1989;158:399-403. [PubMed]
- Laronga C, Kemp B, Johnston D, et al. The incidence of occult nipple-areola complex involvement in breast cancer patients receiving a skin-sparing mastectomy. Ann Surg Oncol 1999;6:609-13. [PubMed]
- Rusby JE, Gui GP. Nipple-sparing mastectomy in women with large or ptotic breasts. J Plast Reconstr Aesthet Surg 2010;63:e754-5. [PubMed]
- Eisenberg RE, Chan JS, Swistel AJ, et al. Pathological evaluation of nipple-sparing mastectomies with emphasis on occult nipple involvement: the Weill-Cornell experience with 325 cases. Breast J 2014;20:15-21. [PubMed]
- Chirappapha P, Petit JY, Rietjens M, et al. Nipple sparing mastectomy: does breast morphological factor related to necrotic complications? Plast Reconstr Surg Glob Open 2014;2:e99. [PubMed]
- Gurtner GC, Jones GE, Neligan PC, et al. Intraoperative laser angiography using the SPY system: review of the literature and recommendations for use. Ann Surg Innov Res 2013;7:1. [PubMed]
- Phillips BT, Lanier ST, Conkling N, et al. Intraoperative perfusion techniques can accurately predict mastectomy skin flap necrosis in breast reconstruction: results of a prospective trial. Plast Reconstr Surg 2012;129:778e-88e. [PubMed]
- Duggal CS, Madni T, Losken A. An outcome analysis of intraoperative angiography for postmastectomy breast reconstruction. Aesthet Surg J 2014;34:61-5. [PubMed]
- Alander JT, Kaartinen I, Laakso A, et al. A review of indocyanine green fluorescent imaging in surgery. Int J Biomed Imaging 2012;2012:940585.
- Komorowska-Timek E, Gurtner GC. Intraoperative perfusion mapping with laser-assisted indocyanine green imaging can predict and prevent complications in immediate breast reconstruction. Plast Reconstr Surg 2010;125:1065-73. [PubMed]
- Petit JY, Veronesi U, Orecchia R, et al. Nipple sparing mastectomy with nipple areola intraoperative radiotherapy: one thousand and one cases of a five years experience at the European institute of oncology of Milan (EIO). Breast Cancer Res Treat 2009;117:333-8. [PubMed]
- Rusby JE, Brachtel EF, Taghian A, et al. George Peters Award. Microscopic anatomy within the nipple: implications for nipple-sparing mastectomy. Am J Surg 2007;194:433-7. [PubMed]
- Moyer HR, Ghazi B, Daniel JR, et al. Nipple-sparing mastectomy: technical aspects and aesthetic outcomes. Ann Plast Surg 2012;68:446-50. [PubMed]
- Peled AW, Foster RD, Esserman LJ, et al. Increasing the time to expander-implant exchange after postmastectomy radiation therapy reduces expander-implant failure. Plast Reconstr Surg 2012;130:503-9. [PubMed]
- Warren Peled A, Foster RD, Stover AC, et al. Outcomes after total skin-sparing mastectomy and immediate reconstruction in 657 breasts. Ann Surg Oncol 2012;19:3402-9. [PubMed]
- Endara M, Chen D, Verma K, et al. Breast reconstruction following nipple-sparing mastectomy: a systematic review of the literature with pooled analysis. Plast Reconstr Surg 2013;132:1043-54. [PubMed]
- Garwood ER, Moore D, Ewing C, et al. Total skin-sparing mastectomy: complications and local recurrence rates in 2 cohorts of patients. Ann Surg 2009;249:26-32. [PubMed]
- Wapnir I, Dua M, Kieryn A, et al. Intraoperative imaging of nipple perfusion patterns and ischemic complications in nipple-sparing mastectomies. Ann Surg Oncol 2014;21:100-6. [PubMed]
- Rivolin A, Kubatzki F, Marocco F, et al. Nipple-areola complex sparing mastectomy with periareolar pexy for breast cancer patients with moderately ptotic breasts. J Plast Reconstr Aesthet Surg 2012;65:296-303. [PubMed]
- Ghali S, Butler PE, Tepper OM, et al. Vascular delay revisited. Plast Reconstr Surg 2007;119:1735-44. [PubMed]
- Jensen JA, Lin JH, Kapoor N, et al. Surgical delay of the nipple-areolar complex: a powerful technique to maximize nipple viability following nipple-sparing mastectomy. Ann Surg Oncol 2012;19:3171-6. [PubMed]
- Palmieri B, Baitchev G, Grappolini S, et al. Delayed nipple-sparing modified subcutaneous mastectomy: rationale and technique. Breast J 2005;11:173-8. [PubMed]


