A cost analysis of thyroid core needle biopsy vs. diagnostic surgery
Introduction
Cytology by fine needle aspiration (FNA) is used worldwide to evaluate both palpable and non-palpable thyroid nodules. It is highly accurate, reproducible, and cost effective (1,2). However, 20% of these biopsies are given the pathologic classification of indeterminate neoplasm (IN). These samples are classified as Thy-3 according to British Thyroid Association guidelines (3), Class 3 by American Association of Clinical Endocrinologists/Association Medici Endocrinology/European Thyroid Association guidelines (1), or Category III-IV using the Bethesda System for Reporting Thyroid Cytopathology (4), with the latter dividing the uncertain reports into two categories of cancer risk. The samples classified as IN represent the gray zone of FNA results, in which cytologic evaluation cannot discriminate benign from malignant neoplasia (5). Traditionally, patients with IN cytology have required diagnostic thyroidectomy (1,2), with about 3 in 4 nodules ultimately being ruled benign (6). A method that will identify these benign nodules can help patients to avoid unnecessary surgery and is therefore highly desirable.
Over the last decade, there has been investigation into potential markers for benign thyroid lesions (6-10). Unfortunately, there are no clinical, molecular, cytologic, ultrasonographic, or scintigraphic features exclusively associated with benign neoplasia; these examinations are useful only for thyroid cancer risk stratification (6-11). Recently, however, core needle biopsy (CNB) has been identified as a highly reliable approach to thyroid diagnosis (12). CNB allows for microhistologic analysis of IN thyroid tissue, a more accurate evaluation than FNA cytology. Up to 98% of IN lesions are able to be classified as malignant or benign when CNB is used for follow-up analysis (13-19), allowing patients with benign nodules to avoid surgery. Although the popularity of CNB has risen worldwide, the potential cost benefit provided by its use has not yet been reported.
Our aim was to analyze the cost effectiveness of using CNB in patients with previous IN pathology on FNA.
Material and methods
Patients
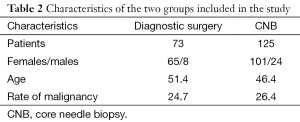
Between January 2012 and December 2013, a consecutive series of 125 patients (101 females, 24 males; mean age, 46.4 years) underwent CNB at Ospedale Israelitico, Rome, Italy. Each patient had a single nodule, and all had previously undergone FNA with a result of IN. All cytologic examinations were conducted by an expert cytopathologist (LG). All microhistologic CNB specimens were evaluated by an experienced pathologist (AC).
During the same period, 73 consecutive patients (65 females, 8 males; mean age, 51.4 years) with IN cytology on FNA underwent diagnostic surgery at the Department of Surgical Sciences, Sapienza University, Rome.
The study was conducted according to the Declaration of Helsinki and was approved by institute ethical committee. Informed consent was obtained by all patients.
Cost analysis
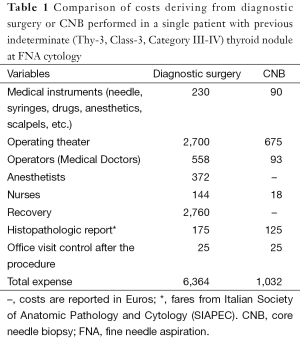
All CNB procedures were performed in the outpatient surgery department. The overall cost for each patient included the price of two cutting needles (45€ each), other surgical instruments, the operating theater, the surgical team, and the cost of microhistologic examination. The cost of diagnostic surgery included all medical instruments and medications used for the procedure, patient recovery costs, the operating theater, the surgical team, and the cost of histologic examination.
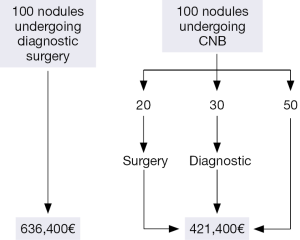
We used our results to construct an ideal series of 100 patients with indeterminate thyroid nodules by FNA in order to estimate the potential impact on expenses of performing CNB vs. diagnostic surgery.
Statistical analysis
Means and standard deviations were compared using t-test. The rate of malignancy recorded in the two groups was compared using the chi-square test. All statistical analyses were performed using Graph Pad Prism (Graph Pad Software Inc., La Jolla, CA, USA).
Results
Core needle biopsy (CNB)
Of the 125 patients with FNA followed by CNB, 53 (42.4%) had benign lesions and were able to avoid surgery. A total of 26 patients (20.8%) had malignancy and were surgically treated. The remaining 46 patients (36.8%) had indeterminate results on CNB and underwent diagnostic surgery. Of these 46, a total of 7 had cancer. The overall rate of malignancy was 26.4% (n=33). The mean cost of CNB for a single nodule was 1,032€ (Table 1). In those patients with malignant or indeterminate results on CNB, the total cost included thyroidectomy.
Full table
Diagnostic surgery
Of the 73 patients who underwent diagnostic surgery, 18 (24.7%) had cancer and 55 (75.3%) had benign lesion. The mean recovery duration was 2.4 days, and the mean expense for each patient was 6,364€ (Table 1).
Comparison of the results
There was no significant difference in the rate of malignancy between the groups (26.4% in the CNB group and 24.7% in the diagnostic surgery group). The mean patient age and nodule size were no different between groups (Table 2). No operative difficulties were recorded in patients undergoing surgery after CNB.
Full table
Impact of CNB on treatment expense
The cost of a single CNB was lower than that of diagnostic surgery (Table 1). To compare the expense, we constructed an ideal cohort of 100 patients with IN cytology on FNA. Of these, 50 nodules would be benign, with patients able to avoid surgery. A total of 20 would be malignant and treated by thyroidectomy, and 30 patients would have indeterminate results on CNB and would require surgery for diagnosis. The total expense incurred by 100 patients submitting to CNB is 33.8% lower than the expense of diagnostic surgery, with a saving of 215,000€ (Figure 1).
Discussion
Cytological indeterminate nodules represent a major dilemma for thyroidologists. These lesions make up about 20% of thyroid cytology results, with 70-80% ultimately being determined benign. A large number of researchers have attempted, unsuccessfully, to discover molecular or clinical markers that are able to predict the likelihood of malignancy in patients with IN (6-11). Traditionally, thyroidectomy has been required to obtain a definite diagnosis, increasing costs in a large number of patients with benign nodules. Recently, CNB has been reported to be highly accurate in identifying the majority of benign nodules with prior uncertain cytology, allowing patients to avoid diagnostic thyroidectomy. This should theoretically reduce the expense associated with treatment. Furthermore, a very good prognosis has been reported for patients with thyroid cancers previously classified as indeterminate at cytology (20,21).
We reviewed a large series (198 patients) with indeterminate cytology that underwent different diagnostic approaches at two institutions. CNB had a much lower cost than routine diagnostic thyroidectomy, reducing the total surgical expense by about one-third. In Italy, 44,000 thyroidectomies are annually performed, with 11,000 of these patients diagnosed with malignancy. We may estimate that about 3,000 nodules are assessed as indeterminate at FNA each year. If all of these patients undergo diagnostic surgery, the cost would be about 19 million Euros; CNB would therefore allow a savings of about 6 million Euros. We did not take into account other expenses and consequences of surgery, such as lost work days, potential postoperative complications, chronic treatment and follow-up of athyreotic patients, and hypocalcaemia. All of these may be avoided if benign pathology is able to be confirmed using CNB.
A combined performance of repeated FNA plus CNB might be considered in indeterminate lesions. Tow relevant studies (16,17) used that in large series of nodules, and the results showed that CNB has higher accuracy than repeated FNA, but the combination of the two biopsies improves the rate of diagnosis. This approach could reduce the number of thyroidectomies and save the expense to manage these patients.
Some limitations of the present study have to be addressed. First, here we reported a series of thyroid nodules enrolled over the period 2012-2013 and classified as indeterminate by current Italian reporting system. More recently, the latter guidelines, in agreement with international ones (4,22), suggested a sub-classification of the indeterminate lesions in two classes (i.e., TIR-3a and TIR-3b) which are associated with different malignancy risk (i.e., <10% and 15-30%, respectively) (23). The results of our study have to be confirmed in these sub-categories. In addition, incidental contralateral thyroid cancer cannot be excluded by CNB of a benign lesion. Also, a patient with a large symptomatic nodule may be selected for surgery regardless of benign results on CNB. Finally, our cost analysis was based on an ideal cohort of 100 patients; a prospective study is needed to confirm our results.
In conclusion, CNB can provide a definitive diagnosis in a large proportion of patients with indeterminate thyroid nodules by FNA cytology. Those patients with benign nodules can therefore avoid diagnostic thyroidectomy. The use of CNB reduces the cost of treatment by about one-third.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gharib H, Papini E, Paschke R, et al. AACE/AME/ETA Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules: executive summary of recommendations. J Endocrinol Invest 2010;33:51-6. [PubMed]
- Cooper DS, Doherty GM, Haugen BR, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2006;16:109-42. [PubMed]
- British Thyroid Association, Royal College of Physicians. Guidelines for the management of thyroid cancer (Perros P, ed) 2nd edition. Report of the Thyroid Cancer Guidelines Update Group. London: Royal College of Physicians, 2007.
- Cibas ES, Ali SZ. The Bethesda System for Reporting Thyroid Cytopathology. Thyroid 2009;19:1159-65. [PubMed]
- Baloch ZW, Sack MJ, Yu GH, et al. Fine-needle aspiration of thyroid: an institutional experience. Thyroid 1998;8:565-9. [PubMed]
- Trimboli P, Treglia G, Guidobaldi L, et al. Clinical characteristics as predictors of malignancy in patients with indeterminate thyroid cytology: a meta-analysis. Endocrine 2014;46:52-9. [PubMed]
- Bartolazzi A, Orlandi F, Saggiorato E, et al. Italian Thyroid Cancer Study Group (ITCSG). Galectin-3-expression analysis in the surgical selection of follicular thyroid nodules with indeterminate fine-needle aspiration cytology: a prospective multicentre study. Lancet Oncol 2008;9:543-9. [PubMed]
- Saggiorato E, De Pompa R, Volante M, et al. Characterization of thyroid 'follicular neoplasms' in fine-needle aspiration cytological specimens using a panel of immunohistochemical markers: a proposal for clinical application. Endocr Relat Cancer 2005;12:305-17. [PubMed]
- Trimboli P, Condorelli E, Catania A, et al. Clinical and ultrasound parameters in the approach to thyroid nodules cytologically classified as indeterminate neoplasm. Diagn Cytopathol 2009;37:783-5. [PubMed]
- Treglia G, Caldarella C, Saggiorato E, et al. Diagnostic performance of (99m)Tc-MIBI scan in predicting the malignancy of thyroid nodules: a meta-analysis. Endocrine 2013;44:70-8. [PubMed]
- Trimboli P, Treglia G, Sadeghi R, et al. Reliability of real-time elastography to diagnose thyroid nodules previously read at FNAC as indeterminate: a meta-analysis. Endocrine 2014. [Epub ahead of print]. [PubMed]
- Trimboli P, Crescenzi A. Thyroid core needle biopsy: taking stock of the situation. Endocrine 2015;48:779-85. [PubMed]
- Park KT, Ahn SH, Mo JH, et al. Role of core needle biopsy and ultrasonographic finding in management of indeterminate thyroid nodules. Head Neck 2011;33:160-5. [PubMed]
- Zhang S, Ivanovic M, Nemcek AA Jr, et al. Thin core needle biopsy crush preparations in conjunction with fine-needle aspiration for the evaluation of thyroid nodules: a complementary approach. Cancer 2008;114:512-8. [PubMed]
- Screaton NJ, Berman LH, Grant JW. US-guided core-needle biopsy of the thyroid gland. Radiology 2003;226:827-32. [PubMed]
- Sung JY, Na DG, Kim KS, et al. Diagnostic accuracy of fine-needle aspiration versus core-needle biopsy for the diagnosis of thyroid malignancy in a clinical cohort. Eur Radiol 2012;22:1564-72. [PubMed]
- Na DG, Kim JH, Sung JY, et al. Core-needle biopsy is more useful than repeat fine-needle aspiration in thyroid nodules read as nondiagnostic or atypia of undetermined significance by the Bethesda system for reporting thyroid cytopathology. Thyroid 2012;22:468-75. [PubMed]
- Nasrollah N, Trimboli P, Guidobaldi L, et al. Thin core biopsy should help to discriminate thyroid nodules cytologically classified as indeterminate. A new sampling technique. Endocrine 2013;43:659-65. [PubMed]
- Nasrollah N, Trimboli P, Rossi F, et al. Patient's comfort with and tolerability of thyroid core needle biopsy. Endocrine 2014;45:79-83. [PubMed]
- Trimboli P, Bongiovanni M, Rossi F, et al. Differentiated thyroid cancer patients with a previous indeterminate (Thy 3) cytology have a better prognosis than those with suspicious or malignant FNAC reports. Endocrine 2015;49:191-5. [PubMed]
- Rago T, Scutari M, Latrofa F, et al. The large majority of 1520 patients with indeterminate thyroid nodule at cytology have a favorable outcome, and a clinical risk score has a high negative predictive value for a more cumbersome cancer disease. J Clin Endocrinol Metab 2014;99:3700-7. [PubMed]
- Perros P, Boelaert K, Colley S, et al. British Thyroid Association. Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf) 2014;81:1-122. [PubMed]
- Nardi F, Basolo F, Crescenzi A, et al. Italian consensus for the classification and reporting of thyroid cytology. J Endocrinol Invest 2014;37:593-9. [PubMed]


