Esophageal recurrence of medullary thyroid carcinoma
Introduction
Medullary thyroid carcinoma (MTC) accounts for about 5% of all thyroid malignant neoplasms. In most cases MTC is sporadic, but in 20-25% it is part of a genetic syndrome (MEN 2A, MEN 2B and familial MTC). For most of the patients, total thyroidectomy, level VI compartmental dissection and lateral neck dissection are the first line treatment. Five-year recurrence-free survival varies between 20-73% and is related to the number of metastatic nodes and postoperative calcitonin and CEA doubling times (1). MTC usually recurs locally but as far as we know there have been no reports on intramural oesophageal recurrences.
Case report
A 38-year-old woman was diagnosed in 2002 with sporadic MTC, on a nodule of the right thyroid lobe. Lateral cervical nodes were positive for metastasis on FNA. Calcitonin levels were 500 pg/mL. A total thyroidectomy, bilateral central compartment dissection, and right modified radical neck dissection (II-V) were performed (Figure 1). The histopathological report revealed nodal metastasis in 15 of the 23 nodes removed from the central compartment and in 8 of the 47 nodes resected from the lateral right compartment (pT1N1b), without extrathyroid extension or extranodal extension. The resection was considered R0 and postoperatively calcitonin dropped to 90 pg/mL.
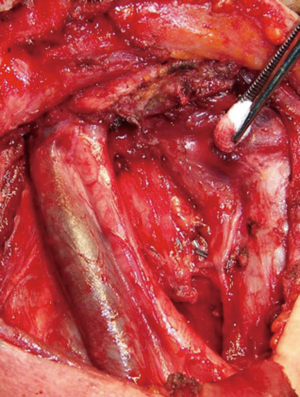
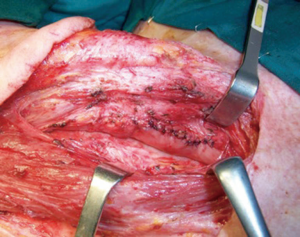
By 2010, the level of calcitonin had raised to 470 pg/mL. Physical examination revealed a subcutaneous lump under the thyroidectomy scar while an ultrasonography identified an enlarged right paratracheal node. After performing a neck-chest-abdomen CT and a PET/CT, there was no evidence of distant metastases. A second surgery was performed and both the subcutaneous nodule and the paratracheal metastatic nodes were resected. The right inferior recurrent laryngeal nerve was infiltrated by the central compartment nodes (Figure 2) and had to be resected. The postoperative level of calcitonin was 461 pg/mL. Later in 2012 subcutaneous nodules reappeared under the scar and were once again resected.

We then lost sight of the patient who requested a second opinion from another centre where a further central neck recurrence was treated with repeated percutaneous ethanol injections.
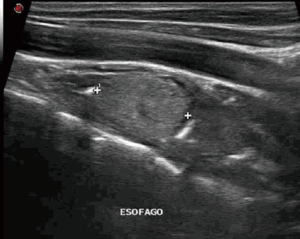
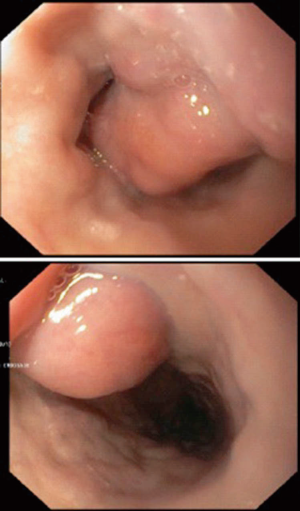
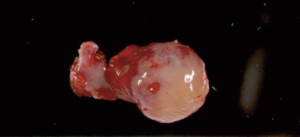
In 2013, the patient was seen again in our unit complaining of dysphagia to solids. Calcitonin was 223 pg/mL. A neck ultrasound revealed two right nodules, probably within the esophageal wall (Figure 3). An upper gastrointestinal endoscopy found two submucosal nodules in the cervical oesophagus (Figure 4). The patient underwent a resection of the right lateral esophageal wall. There was no evidence of locoregional recurrence (Figure 5). Histopathology revealed that both nodules were metastases of MTC located in the submucosal layer of esophagus. There was no infiltration of the muscle layer (Figure 6). After surgery, calcitonin dropped to 89 pg/mL and was 155 pg/mL 1 year later during the follow-up (doubling time >1 year).
Discussion
MTC is known to give metastases via the lymphatic system to locoregional nodes and by hematogenous spread causing distant metastases to the lungs, liver and bones (1). Only a few cases of thyroid carcinoma metastases, mainly of follicular or papillary carcinoma, have been described to occur in the pharyngoesophageal axis. Even fewer of these cases describe limited metastases to the esophagus (2,3). The implantation of papillary or follicular carcinoma cancerous cells has been described a number of times after fine needle biopsy and other invasive procedures (4). This process has been associated with multiple factors such as needle size, number of passages during biopsy, excessive suction, needle withdrawal without releasing suction, and injection of tumour cells during biopsy.
To the best of our best knowledge, there has only been one other case of MTC metastasis to the upper GI tract involving the epiglottis (5). In this case, a 50-year-old woman who had initially undergone total thyroidectomy for MTC had developed mild dyspnea. Laryngoscopy found small nodular formations in the larynx. These were resected using CO2-laser, with the pathological diagnosis of metastatic MTC.
In our case, the submucosal location of the esophageal nodules, with an uninfiltrated muscular layer suggests metastatic origin of the disease rather than locoregional spread. Yet we cannot exclude the possibility that MTC cells were implanted into the esophageal wall by percutaneous ethanol injections or fine needle biopsy. However, there have been no reports of intraesophageal metastatic implants after these specific procedures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Meijer JA, le Cessie S, van den Hout WB, et al. Calcitonin and carcinoembryonic antigen doubling times as prognostic factors in medullary thyroid carcinoma: a structured meta-analysis. Clin Endocrinol (Oxf) 2010;72:534-42. [PubMed]
- Lee B, Cook G, John L, et al. Follicular thyroid carcinoma metastasis to the esophagus detected by 18FDG PET/CT. Thyroid 2008;18:267-71. [PubMed]
- Wisotzki C, Friese M, Ehresmann J, et al. Esophageal metastasis from papillary thyroid cancer: diagnosis by 131I SPECT/CT. Clin Nucl Med 2014;39:e73-4. [PubMed]
- Moon HJ, Park SH, Hong SW, et al. Extrathyroidal implantation of thyroid tumor cells after needle biopsy and other invasive procedures. Thyroid 2010;20:459-64. [PubMed]
- Desuter G, Schmitz S, Jamar F, et al. Pharyngoesophagolaryngeal metastases of medullary thyroid carcinoma. A case report. Ann Endocrinol (Paris) 2003;64:448-52. [PubMed]