The pros and cons of routine central compartment neck dissection for clinically nodal negative (cN0) papillary thyroid cancer
Introduction
Although thyroid cancers represent approximately 1% of all new cancer diagnoses in the United States each year, it is the most common endocrine related cancer (1). The American Cancer Society estimated that approximately 44,670 new cases of thyroid cancer would be diagnosed in 2010. The overall incidence has risen from 1.3/100,000 for women and 4.6/100,000 for men in the year 1935 to 16.3/100,000 for women and 5.6/100,000 for men in 2008 (2). The age & gender adjusted incidence has increased faster than that of any other malignancy in the recent years, with the majority of this increase belonging to small papillary thyroid carcinoma (PTC) (3).
Epidemiology
Thyroid cancers are divided into PTCs (80%), follicular thyroid carcinomas (FTCs) (10%), medullary thyroid carcinomas (5-10%) and anaplastic thyroid carcinomas (1-2%). Primary lymphomas and sarcomas are rare (1). PTC and FTC make up the well-differentiated thyroid carcinomas. The prognosis of the differentiated thyroid carcinomas (DTC) is generally excellent. Ten-year relative survival rates in a large cohort of United States patients with papillary and follicular cancer were, respectively, 93% and 85% (4). In one cohort study, 40 years recurrence rates were about 35%, two thirds of which occurred within the first decade after initial therapy. Thirty years cancer mortality rates were about 12% with local recurrence and 43% with distant recurrence (5).
DTC
PTC is the most common type of differentiated thyroid carcinoma. It is well known as a lymphotropic type of cancer and thus has high tendency to metastasize to regional lymph nodes (LNs) (6). Clinically evident nodal disease is present in approximately 5 to 10 percent of patients with PTC and a preoperative neck ultrasound can detect LN disease in up to 30 percent of patients (7-10). In contrast, less than five percent of patients with FTC develop nodal metastatic disease; the hematogenous rather than the lymphatic route is the primary pathway for metastasis (11). The prognosis of FTC is related to the age on presentation and the degree of capsular with or without vascular invasion. The diagnosis of FTC cannot always be made at the time of initial surgery. Prophylactic central neck dissection (pCND) during the first operation is of no value in FTC because the diagnosis of cancer is not established at that moment and also it tends not to spread via the lymphatic route.
Central neck dissection (CND) for PTC at the time of total thyroidectomy (TT)
The availability of non-invasive ultrasound and fine needle aspiration has led to detection of PTC in early stage. Higher incidence of small thyroid nodule with unknown cervical LNs status has posed a new management challenge to clinicians. Despite the excellent prognosis, many patients with PTC will develop nodal metastases in the central neck (level VI) or lateral neck (levels II, III, and IV) at the time of presentation or during the course of follow-up.
The guideline from the National Comprehensive Cancer Network recommends CND only in the presence of clinically nodal disease. Similarly, the current standard of care for thyroid cancer based on the consensus guideline from American Thyroid Association (ATA), includes TT and a “therapeutic” LN dissection for patients with clinical evidence of nodal disease or a “prophylactic” CND in patients with a tumor more than 4 cm (T3 or T4 tumor) even in the absence of clinical evidence of nodal involvement (3). Most endocrine surgeons agree that compartment-based nodal dissection is appropriate for enlarged LNs that are identified on preoperative or during intraoperative inspection and palpation. However, substantial controversy still exists regarding the role of “prophylactic” neck dissection for patients with PTC.
The neck dissection is defined by ATA as compartment oriented removal of all the lymphatic tissue with the fibroadipose tissue en bloc within the neck while preserving critical structures. A pCND is defined as resection of level VI LNs that appear normal in preoperative imaging and intra-operative assessment. Anatomical neck level VI or central compartment of the neck refers to the LNs that located between the carotid arteries from the innominate artery to the hyoid bone, includes the pretracheal, prelaryngeal and parartracheal LNs (3).
In general, cervical nodal metastasis tends to spread in a stepwise fashion from the thyroid to the ipsi-lateral central (level VI), then to the lateral compartment (level II to V) and/or contra-lateral central compartment. Therefore, the central compartment is considered to be the first echelon of nodal metastasis in thyroid cancer. Theoretically, removal of central LNs may alter the prognosis of thyroid cancer especially in PTC. Many endocrine surgeons have advocated pCND in their patient without clinical or radiographic evidence of LN involvement at the time of TT (12). The actual role of pCND in thyroid cancer remains a major topic of debate. This article aimed to review the arguments for and against pCND in PTC.
Arguments for pCND in clinically nodal negative (cN0) PTC
- Metastatic disease to central compartment LNs is frequently identified in patients with PTC. Nodal disease is an important issue in managing patients with thyroid cancer. According to ATA, LN metastasis is present in up to 20-50% of the patients undergoing an elective node dissection for PTC and up to 90 percent of patients will have microscopic metastatic disease (13,14). Sergio Zuniga et al. demonstrated that in 136 patients who underwent pCND, 82.3% (112 patients) had metastatic LNs (15). Similar conclusion was drawn by Roh et al. in which 51 (62.2%) out of 82 patients with neck dissection had LN metastases in the central neck compartment (16). Therefore, there were significant numbers of patients undergoing TT for cN0 PTC without pCND are likely to have occult nodal disease left behind in the neck.
- Some studies have raised the possibility that failure to remove tumour bearing cervical LN could be detrimental in patient with PTC. Cervical LN metastasis is associated with higher risk of disease recurrence and cancer mortality. This is supported by the following studies:
- In a retrospective review by Wada et al., among 134 patients with papillary thyroid cancer undergoing TT with neck dissection, 17 patients (12.7%) developed local recurrence in cervical LNs. Recurrence rate was significantly higher for patients undergoing a therapeutic neck dissection for suspicious lymphadenopathy (n=42) when compared to patients undergoing an elective neck dissection (END) with no lymphadenopathy [23.8% (10 patients) versus 7.6% (7 patients)]. Microscopic disease was identified in 62 of 92 patients (67.4%) undergoing an END. Of the 62 patients with microscopic nodal disease, the local recurrence rate was 11.3%. Of the 30 patients with histologically negative nodes, there were no local recurrences. Of the 104 patients with histologically positive nodes, the local recurrence rate was 16.3%. Thus, he concluded that lymphadenopathy and microscopic nodal status were significantly associated with recurrences and disease free survival rates (17).
- In a Cox regression model, studied of 1,355 patients with 30 years of follow-up, the likelihood of cancer death was increased by regional lymph-node metastases in patients without distant metastases (18).
- Additional data from Surveillance Epidemiology and End Results database comprising 19,918 patients showed that for those with LN metastasis, the 14-year survival rate was 79% and was 82% in non-metastatic patients (P<0.05) (19).
- Ultrasound neck and aspiration cytology are currently the preferred investigation tools for evaluation of the thyroid and cervical LN. However, detection of central compartment LN metastasis using ultrasound remains difficult even in expert hand because the abnormal central LNs are often small in size and frequently located deep inside the neck or just posterior to the sternum (29-31), where the overlying thyroid gland often hinders adequate visualization (32).
- A detectable post-operation Thyroglobulin (Tg) level is a surrogate marker of persistent or recurrent thyroid cancer after TT and RAI ablation. Prophylactic CND results in a higher rate of stimulated athyroglobulinemia after surgery. Hence, it could facilitate follow up and cancer surveillance of the neck. The relation between pCND and Tg was illustrated by the following studies:
- Sywak et al. examined 447 patients with clinically node-negative PTC. 56 patients underwent TT plus pCND. There was a significantly lower level of stimulated Tg at six months after RAI ablation (mean: 0.4 versus 9.3 mg/L, P<0.02) and higher proportion of athyroglobulinemia (72% versus 43%; P<0.001) (26).
- In a study compared serum Tg level in 113 patients underwent TT alone with 119 patients underwent TT in conjunction with pCND bilaterally: the post-operative Tg was significantly less in pCND group (1.07 vs. 2.24 ng/mL respectively; P=0.022). However, the two groups became similar after low dose radioactive iodine treatment (0.44 vs. 0.69 ng/mL respectively; P=0.341). There was also no significant difference in three years local-regional control rate in both the studied groups (98.35% vs. 96.5%; P=0.368). Thus, he concluded that pCND lower the serum Tg level but is not helpful in decreasing short term recurrence in patient with cN0 PTC (20).
- Lang et al. analysed 185 patients with PTC retrospectively. In this study, 82 (44.3%) patients underwent unilateral TT with pCND and found that this group of patient has lower median pre-ablative-stimulated Tg level (<0.5 versus 6.7 μg/L, P<0.001) and achieved a higher rate of pre-ablative athyroglobulinemia (51.2% versus 22.3%, P=0.024) than those who underwent a TT only. However, these differences were not observed six months after ablation (31). The most likely explanation for this difference was that the residual microscopic disease was ablated by RAI ablation subsequently. Thus, the group without pCND achieved similar stimulated Tg levels and similar rate of athyroglobulinemia six months after ablation (36).
- Thyroid cancer patients without pCND are at higher risk of neck recurrence which may require second operation. Re-operation is associated with a higher morbidity than pCND when done at the time of initial TT. Complications such as iatrogenic injuries of the nerve and parathyroid gland would be higher in re-operative central lymph node dissection (CLND) because of the scarring in the operative field and distorted anatomy in the central neck after TT. For example, Segal et al. who had reviewed 503 patients retrospectively found that reoperation had a significantly higher complication rate of permanent recurrent nerve injury (25% versus 5.8%) and hypoparathyroidism (8.3% versus 5.0%) compared with primary operation (39). Other studies also revealed similar outcomes (40-43). It is reasonable to dissect LNs in the central compartment routinely, because subsequent surgery for node metastases in this area poses more difficulties. On the other hand, Shen et al. argued that neck reoperation could also be performed as safely as first operation by an “experienced” surgeon. In his study, the initial and re-operative CLND had similar complication and recurrence rates (44).
Based on the above findings, there are potential benefits of lower recurrence in those who underwent pCND. Table 1 summarizes the local regional recurrence rates between those underwent TT with prophylactic neck dissection and those who underwent TT alone.
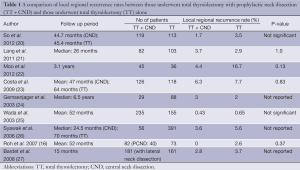
Full table
In contrast, a recent meta-analysis by Zetoune et al., comprising five retrospective comparative studies (n=1,264), found that there was an “insignificant” trend toward lower overall recurrence rate in the group who underwent either unilateral or bilateral pCND when compared to those who had TT only (2.02% versus 3.92%, odds ratio =1.05, 95% CI, 0.48-2.31) (28). Furthermore, people may argue that the subclinical LN metastasis could be ablated by radioactive iodine post operation. But, it is worth noting that not all tumours will respond to RAI ablation.
Kim et al. found that preoperative ultrasound has an accuracy of 77% only in detection of LN metastasis. Despite the fact that ultrasound has high specificity of 92% and positive predictive value of 81%, the sensitivity is only 51% and the negative predictive value is 76% (33,34). Other sophisticated imaging modalities such as computer tomography and magnetic resonance imaging have not shown any additional advantage, they are more beneficial in patients with extensive nodal involvement. Because of the lymphadenopathy cannot be reliably assessed by imaging studies, pCND has been advocated. Prophylactic CND allows histology examination of LNs and more accurate pathological staging.
Wang et al. reviewed 49 patients (48%) who were cN0 PTC and found that pCND resulted in detection of unsuspected metastasis lymphadenopathy in 20 (41%) of patients and changed RAI recommendation in 14 (33%) of patients (35). Similarly, in a study performed in our hospital, of 82 patients underwent pCND, 17.1% were upstaged from stage I/II to stage III due to detection of nodal metastasis after surgery (21).
Unlike the above studies, no difference was found by Raffaelli M et al. concerning mean post-operative basal and stimulated Tg after a prospective evaluation of total 186 patients with cN0 underwent TT with or without; ipsi- or bilateral CND (37). Similarly, Hughes et al. also found that there was no difference in post-ablation median- stimulated Tg level or rate of athyroglobulinemia between patients underwent TT with or without bilateral pCND (38).
Arguments against pCND in cN0 PTC
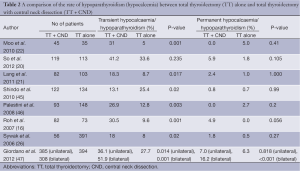
- The most frequently quoted data arguing against the need for routine pCND is increased risk of transient hypoparathyroidism. Risk of transient hypocalcemia has been consistently shown in many studies (Table 2).
- Moo et al. found that the rates of temporary hypocalcemia were higher in CND group compared to no neck dissection group (31% versus 5 %; P=0.01). Interestingly, the rate of permanent hypocalcemia were the same (5% versus 0%; P=0.41) (22).
- A meta-analysis found that patients with pCND were almost 2.5 times more likely to have temporary hypocalcemia than those who underwent TT alone (26.0% vs. 10.8%; OR=2.56; 95% CI: 1.75-2.57) (48).
- So et al. reviewed 232 patients who underwent surgery for clinically node negative papillary thyroid micro-carcinoma from 1999 to 2006, reported that the frequency of permanent hypocalcemia was approximately 3 times greater in TT with pCND (5.9%) than TT only (1.8%) although this finding did not reach statistical significance (20).
- A recent systematic review of five retrospective studies, evaluated the morbidity of pCND and found that there was one extra case of transient hypocalcaemia for every eight pCNDs performed (49). However, there was no increased risk of permanent hypocalcaemia and recurrent laryngeal nerve injury. The higher rate of temporary hypoparathyroidism could be explained by the higher chance of unintentional removal or devascularisation of parathyroid glands during dissection.
- LN involvement in papillary thyroid cancer can be macroscopic (identified on preoperative imaging or intraoperative inspection) or microscopic (identified on pathologic review only). Macroscopic LN involvement is associated with a significant higher rate of local recurrence (10-42%) (54,55). It is unknown what the natural history is, in PTC with only microscopic LN involvement/subclinical nodal metastasis.
- In another data presented by Wada et al. on 259 patients with papillary microcarcinoma of thyroid, of mean 53 months follow up, LN metastasis was frequent in the pCND group (60.9%) for central compartment and 39.5% for ipsilateral lateral compartment. While, only 0.43% patient underwent prophylactic neck dissection developed recurrence despite high microscopic LN involvement (25). The nodal recurrence did not differ between the pCND group and the no-dissection group (0.43% vs. 0.65%).
- Gemsenjäger et al. reported a similar finding in their study of 159 patients with PTC and concluded that the rate of occult nodal disease was relatively low and it did not frequently progress to clinical recurrent disease (24).
- There is also little evidence to show that pCND improves cancer-specific survivals in “cN0 PTC”.
- A survical benefit for pCND in DTC was suggested in a study carried out by Tisell et al. (58). They evaluated 175 patients who underwent TT with CND and compared with contemporaneous controls from two other studies conducted on patients in Norway and Finland (59,60). They showed that patients who underwent TT with pCND had a higher survival rate (1.6% versus 8.4-11.1%). However, this study was limited by lack of statistical comparison between the studies.
- In the retrospective review of 244 patients by Costa et al., found that central neck metastasis was predictive of disease recurrent but not influencing the prognosis. The overall recurrence rate in his paper was 6.35 % (8/126; mean follow-up of 47 months) in TT plus pCND group and 7.7% (9/118; mean follow-up of 64 months) in TT alone group (P=0.83). Of those underwent pCND, 47% were diagnosed pN1a but there was no difference in survival rate statistically (23).
- Additional finding came from a cohort analysis of 266 patients with 6.3 years mean follow up and the study reported that the 5-year disease-free survival was comparable; 88.2% in the CND group versus 85.6% in the group that did not undergo CND (P=0.72) (15). Absented of survival benefit with more extensive surgery and longer operation time have limited the routine application of pCND (24).
- The number of positive cervical LNs could affect the disease stage. Prophylactic CND provides more accurate pathological staging and hence, greater incidence of N1a is found. In a study conducted by our hospital demonstrated that 17.1% of 82 patients were upstage from stage I/II to III after pCND (21). Basically, the pathological staging of the tumour for patients aged more than 45 years old are changed to higher stage III (AJCC/UICC TNM staging system) even without any extra-thyroidal extension or other poor prognostic factors (61,62). The outcome of stage migration will be reflected in the overall cancer-specific survival rate. Confusion may occur as they would be classified as stage III with lower 10-year survival (85-90%) while those patients younger than 45 would still remain as stage I with 10-year survival rates of more than 95% (31,61-64).
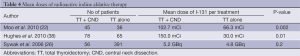
- Because of upstaging, more patients would receive RAI ablation and higher doses of RAI, which might not be necessary in certain patients. In a retrospective study, Hughes et al. had observed that patients in the TT plus pCND group received significantly higher dose of RAI than those in the TT group (150 vs. 30 mCi, P=0.01). Despite a higher dose of RAI, there was no difference in central neck recurrence between TT plus pCND and TT alone group. The author concluded that pCND allows stratification of patient to receive higher doses of RAI but not affected the local recurrence rate (38). Table 4 revealed the published series of doses of I-131 used during RAI ablation. pCND increased LN positivity and has encouraged higher usage of RAI. This is foreseeable that increase of health care costs will be one of the major concerns in the future.
Full table
Prophylactic CND also contributes to the higher rate of temporary recurrent laryngeal nerve injury in a study by Shindo et al. (45) (Table 3). Palestini et al. reported four times higher rate of transient recurrent laryngeal nerve injury in patients underwent TT plus bilateral neck dissection (1.4% versus 5.4%, P=0.059), although it was not statistically significant (46). To date, no studies have shown an increase risk of “permanent” recurrent laryngeal nerve injury in patient underwent pCND. A good example was a study by Giordano et al. as shown in Table 3 (47).
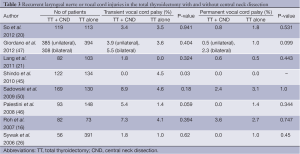
Full table
In general, surgical morbidity correlates with the extent of surgical dissection and the operation skill of surgeons. Since the risks of transient complications are high, especially when performed by low volume surgeons (fewer than 50 cases/year), a selective approach should be considered by determine which patients are likely required pCND pre-operatively and the experience of the surgeon (51).
Several studies described the risk factors that associated with LN metastasis in PTC but the results were inconsistent (46,52,53). In a study by So et al., the male gender, tumour multi-focality and extra-thyroidal extension were independently predictive of subclinical central LN metastasis. It was recommended that patient with these features should be considered for pCND (52). However, realistically only male sex is known preoperatively. Some researchers also believed that large tumour size, patients who have decreased capacity for RAI and those with BRAF mutation should be undergoing pCND at the time of TT (36). Alternatively, suspected LN that found intra-operatively may be confirmed by frozen section examination before proceeding to neck dissection.
Studies have shown that only subclinical metastatic LNs would be identified at the time of pCND for small PTC (56). Wada et al. studied microscopic regional LN status in 92 patients with PTC underwent pCND and found that only few nodes (mean 2.7 nodes/17.8%) were involved pathologically when there was no lymphadenopathy clinically (31). Besides, Vergez et al. also found in their study that most of these pathologically involved LN were subclinical and less that 5 mm in size (66%) (57). With the advances of radio-active iodine ablation, these micrometastasis wouldn’t ultimately result in poorer prognosis. Additionally, it is doubtful that this subclinical occult LN metastasis would eventually develop into clinically significant recurrences in the future.
In summary, for patients harbouring central neck compartment “micrometastasis”, pCND dissection may only provide a limited benefit in terms of reducing recurrence. Routine CND targeted at subclinical LN metastasis has little prognostic benefit. Unnecessary CND will prolong operation time and increase surgical complications.
Full table
Although the treatments with 131-I are generally safe and well-tolerated, patients would still be subjected to potential short- and long-term side-effect of RAI. RAI is contraindicated in patients who are pregnant or breastfeeding. Men who receive RAI treatment for thyroid cancer may have decreased sperm counts and temporary infertility for a period of roughly two years (65,66). Furthermore, Lee et al. found that nausea, vomiting, ageusia (loss of taste), salivary gland swelling, sialoadenitis associated xerostomia, dental caries, pulmonary fibrosis, naso-lacrimal outflow obstruction, and, more importantly, increased risk of second primary malignancies are associated with radioiodine therapy (67,68). I-131 is preferentially taken up by normal and malignant thyroid follicular cells, but it is also accumulated in the stomach, salivary glands, colon, and bladder; salivary glands and breast tissue contain sodium iodide transporters. The risk of salivary gland, breast, bladder and gastrointestinal cancers can theoretically increase in thyroid cancer patients treated with radioiodine. The risk is typically more prominent between two and ten years after therapy with a prevalence of about 0.5% (65,66).
Conclusions
The extent of dissection in the neck is a balance between the greater morbidity of a more extensive neck dissection and the possibility of leaving residual untreated metastatic LN. There is little good evidence (level II or better) to justify pCND in all cN0 PTC. Our review has summarized the conflicting recommendations in which the applicability to clinical practice remains questionable. Further studies in this controversial subject are much needed.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Sharma PK. Thyroid cancer. Medscape Medical News [serial online]. Sep 9, 2013; Accessed August 1, 2013. Available online: http://emedicine.medscape.com/article/851968
- Michael TR. Overview of papillary thyroid cancer. UpToDate [serial online]. May 24, 2013; Accessed August 1, 2013. Available online: http://www.uptodate.com/
- American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, Cooper DS, Doherty GM, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167-214. [PubMed]
- Hundahl SA, Fleming ID, Fremgen AM, et al. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985-1995 Cancer 1998;83:2638-48. [PubMed]
- Mazzaferri EL, Kloos RT. Clinical review 128: Current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab 2001;86:1447-63. [PubMed]
- Sippel RS. Central and lateral compartment lymphadenectomy (neck dissection) for differentiated thyroid cancer. UpToDate [serial online]. March 21, 2013; Accessed August 1, 2013. Available online: http://www.uptodate.com/contents/central-and-lateral-compartment-lymphadenectomy-neck-dissection-for-differentiated-thyroid-cancer
- Grubbs EG, Evans DB. Role of lymph node dissection in primary surgery for thyroid cancer. J Natl Compr Canc Netw 2007;5:623-30. [PubMed]
- Ito Y, Uruno T, Nakano K, et al. An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid 2003;13:381-7. [PubMed]
- Kim E, Park JS, Son KR, et al. Preoperative diagnosis of cervical metastatic lymph nodes in papillary thyroid carcinoma: comparison of ultrasound, computed tomography, and combined ultrasound with computed tomography. Thyroid 2008;18:411-8. [PubMed]
- Stulak JM, Grant CS, Farley DR, et al. Value of preoperative ultrasonography in the surgical management of initial and reoperative papillary thyroid cancer. Arch Surg 2006;141:489-94; discussion 494-6. [PubMed]
- Zaydfudim V, Feurer ID, Griffin MR, et al. The impact of lymph node involvement on survival in patients with papillary and follicular thyroid carcinoma. Surgery 2008;144:1070-7; discussion 1077-8. [PubMed]
- Pisello F, Geraci G, Lo Nigro C, et al. Neck node dissection in thyroid cancer. A review. G Chir 2010;31:112-8. [PubMed]
- Arturi F, Russo D, Giuffrida D, et al. Early diagnosis by genetic analysis of differentiated thyroid cancer metastases in small lymph nodes. J Clin Endocrinol Metab 1997;82:1638-41. [PubMed]
- Cooper DS, Doherty GM, Haugen BR, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2006;16:109-42. [PubMed]
- Zuniga S, Sanabria A.. Prophylactic central neck dissection in stage N0 papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 2009;135:1087-91. [PubMed]
- Roh JL, Park JY, Park CI. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 2007;245:604-10. [PubMed]
- Wada N, Suganuma N, Nakayama H, et al. Microscopic regional lymph node status in papillary thyroid carcinoma with and without lymphadenopathy and its relation to outcomes. Langenbecks Arch Surg 2007;392:417-22. [PubMed]
- Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 1994;97:418-28. [PubMed]
- Podnos YD, Smith D, Wagman LD, et al. The implication of lymph node metastasis on survival in patients with well-differentiated thyroid cancer. Am Surg 2005;71:731-4. [PubMed]
- So YK, Seo MY, Son YI. Prophylactic central lymph node dissection for clinically node-negative papillary thyroid microcarcinoma: influence on serum thyroglobulin level, recurrence rate, and postoperative complications. Surgery 2012;151:192-8. [PubMed]
- Lang BH, Wong KP, Wan KY, et al. Impact of routine unilateral central neck dissection on preablative and postablative stimulated thyroglobulin levels after total thyroidectomy in papillary thyroid carcinoma. Ann Surg Oncol 2012;19:60-7. [PubMed]
- Moo TA, McGill J, Allendorf J, et al. Impact of prophylactic central neck lymph node dissection on early recurrence in papillary thyroid carcinoma. World J Surg 2010;34:1187-91. [PubMed]
- Costa S, Giugliano G, Santoro L, et al. Role of prophylactic central neck dissection in cN0 papillary thyroid cancer. Acta Otorhinolaryngol Ital 2009;29:61-9. [PubMed]
- Gemsenjäger E, Perren A, Seifert B, et al. Lymph node surgery in papillary thyroid carcinoma. J Am Coll Surg 2003;197:182-90. [PubMed]
- Wada N, Duh QY, Sugino K, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 2003;237:399-407. [PubMed]
- Sywak M, Cornford L, Roach P, et al. Routine ipsilateral level VI lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer. Surgery 2006;140:1000-5; discussion 1005-7. [PubMed]
- Bardet S, Malville E, Rame JP, et al. Macroscopic lymph-node involvement and neck dissection predict lymph-node recurrence in papillary thyroid carcinoma. Eur J Endocrinol 2008;158:551-60. [PubMed]
- Zetoune T, Keutgen X, Buitrago D, et al. Prophylactic central neck dissection and local recurrence in papillary thyroid cancer: a meta-analysis. Ann Surg Oncol 2010;17:3287-93. [PubMed]
- Marshall CL, Lee JE, Xing Y, et al. Routine pre-operative ultrasonography for papillary thyroid cancer: effects on cervical recurrence. Surgery 2009;146:1063-72. [PubMed]
- Hwang HS, Orloff LA. Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer. Laryngoscope 2011;121:487-91. [PubMed]
- Wada N, Masudo K, Nakayama H, et al. Clinical outcomes in older or younger patients with papillary thyroid carcinoma: impact of lymphadenopathy and patient age. Eur J Surg Oncol 2008;34:202-7. [PubMed]
- Leboulleux S, Girard E, Rose M, et al. Ultrasound criteria of malignancy for cervical lymph nodes in patients followed up for differentiated thyroid cancer. J Clin Endocrinol Metab 2007;92:3590-4. [PubMed]
- Kim E, Park JS, Son KR, et al. Preoperative diagnosis of cervical metastatic lymph nodes in papillary thyroid carcinoma: comparison of ultrasound, computed tomography, and combined ultrasound with computed tomography. Thyroid 2008;18:411-8. [PubMed]
- Roh JL, Park JY, Kim JM, et al. Use of preoperative ultrasonography as guidance for neck dissection in patients with papillary thyroid carcinoma. J Surg Oncol 2009;99:28-31. [PubMed]
- Wang TS, Evans DB, Fareau GG, et al. Effect of prophylactic central compartment neck dissection on serum thyroglobulin and recommendations for adjuvant radioactive iodine in patients with differentiated thyroid cancer. Ann Surg Oncol 2012;19:4217-22. [PubMed]
- Wong KP, Lang BH. The role of prophylactic central neck dissection in differentiated thyroid carcinoma: issues and controversies. J Oncol 2011;2011:127929.
- Raffaelli M, De Crea C, Sessa L, et al. Prospective evaluation of total thyroidectomy versus ipsilateral versus bilateral central neck dissection in patients with clinically node-negative papillary thyroid carcinoma. Surgery 2012;152:957-64. [PubMed]
- Hughes DT, White ML, Miller BS, et al. Influence of prophylactic central lymph node dissection on postoperative thyroglobulin levels and radioiodine treatment in papillary thyroid cancer. Surgery 2010;148:1100-6; discussion 1006-7. [PubMed]
- Segal K, Friedental R, Lubin E, et al. Papillary carcinoma of the thyroid. Otolaryngol Head Neck Surg 1995;113:356-63. [PubMed]
- Simon D, Goretzki PE, Witte J, et al. Incidence of regional recurrence guiding radicality in differentiated thyroid carcinoma. World J Surg 1996;20:860-6; discussion 866. [PubMed]
- Moley JF, Lairmore TC, Doherty GM, et al. Preservation of the recurrent laryngeal nerves in thyroid and parathyroid reoperations. Surgery 1999;126:673-7; discussion 677-9. [PubMed]
- Kim MK, Mandel SH, Baloch Z, et al. Morbidity following central compartment reoperation for recurrent or persistent thyroid cancer. Arch Otolaryngol Head Neck Surg 2004;130:1214-6. [PubMed]
- Uruno T, Miyauchi A, Shimizu K, et al. Prognosis after reoperation for local recurrence of papillary thyroid carcinoma. Surg Today 2004;34:891-5. [PubMed]
- Shen WT, Ogawa L, Ruan D, et al. Central neck lymph node dissection for papillary thyroid cancer: comparison of complication and recurrence rates in 295 initial dissections and reoperations. Arch Surg 2010;145:272-5. [PubMed]
- Shindo M, Stern A.. Total thyroidectomy with and without selective central compartment dissection: a comparison of complication rates. Arch Otolaryngol Head Neck Surg 2010;136:584-7. [PubMed]
- Palestini N, Borasi A, Cestino L, et al. Is central neck dissection a safe procedure in the treatment of papillary thyroid cancer? Our experience. Langenbecks Arch Surg 2008;393:693-8. [PubMed]
- Giordano D, Valcavi R, Thompson GB, et al. Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid 2012;22:911-7. [PubMed]
- Lang BH, Ng SH, Lau LL, et al. A systematic review and meta-analysis of prophylactic central neck dissection on short-term locoregional recurrence in papillary thyroid carcinoma after total thyroidectomy. Thyroid 2013;23:1087-98. [PubMed]
- Chisholm EJ, Kulinskaya E, Tolley NS. Systematic review and meta-analysis of the adverse effects of thyroidectomy combined with central neck dissection as compared with thyroidectomy alone. Laryngoscope 2009;119:1135-9. [PubMed]
- Sadowski BM, Snyder SK, Lairmore TC. Routine bilateral central lymph node clearance for papillary thyroid cancer. Surgery 2009;146:696-703; discussion 703-5. [PubMed]
- Sippel RS, Chen H. Controversies in the surgical management of newly diagnosed and recurrent/residual thyroid cancer. Thyroid 2009;19:1373-80. [PubMed]
- So YK, Son YI, Hong SD, et al. Subclinical lymph node metastasis in papillary thyroid microcarcinoma: a study of 551 resections. Surgery 2010;148:526-31. [PubMed]
- Roh JL, Park JY, Park CI. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 2007;245:604-10. [PubMed]
- Randolph GW, Duh QY, Heller KS, et al. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid 2012;22:1144-52. [PubMed]
- Moreno MA, Edeiken-Monroe BS, Siegel ER, et al. In papillary thyroid cancer, preoperative central neck ultrasound detects only macroscopic surgical disease, but negative findings predict excellent long-term regional control and survival. Thyroid 2012;22:347-55. [PubMed]
- Randolph GW. Papillary cancer nodal surgery and the advisability of prophylactic central neck dissection: primum, non nocere. Surgery 2010;148:1108-12. [PubMed]
- Vergez S, Sarini J, Percodani J, et al. Lymph node management in clinically node-negative patients with papillary thyroid carcinoma. Eur J Surg Oncol 2010;36:777-82. [PubMed]
- Tisell LE, Nilsson B, Mölne J, et al. Improved survival of patients with papillary thyroid cancer after surgical microdissection. World J Surg 1996;20:854-9. [PubMed]
- Kukkonen ST, Haapiainen RK, Franssila KO, et al. Papillary thyroid carcinoma: the new, age-related TNM classification system in a retrospective analysis of 199 patients. World J Surg 1990;14:837-41; discussion 841-2. [PubMed]
- Salvesen H, Njølstad PR, Akslen LA, et al. Papillary thyroid carcinoma: a multivariate analysis of prognostic factors including an evaluation of the p-TNM staging system. Eur J Surg 1992;158:583-9. [PubMed]
- Shindo M, Wu JC, Park EE, et al. The importance of central compartment elective lymph node excision in the staging and treatment of papillary thyroid cancer. Arch Otolaryngol Head Neck Surg 2006;132:650-4. [PubMed]
- Lang B, Lo CY, Chan WF, et al. Restaging of differentiated thyroid carcinoma by the sixth edition AJCC/UICC TNM staging system: stage migration and predictability. Ann Surg Oncol 2007;14:1551-9.
- Lang BH, Lo CY, Chan WF, et al. Prognostic factors in papillary and follicular thyroid carcinoma: their implications for cancer staging. Ann Surg Oncol 2007;14:730-8. [PubMed]
- Lang BH, Chow SM, Lo CY, et al. Staging systems for papillary thyroid carcinoma: a study of 2 tertiary referral centers. Ann Surg 2007;246:114-21. [PubMed]
- Luster M, Clarke SE, Dietlein M, et al. Guidelines for radioiodine therapy of differentiated thyroid cancer. Eur J Nucl Med Mol Imaging 2008;35:1941-59. [PubMed]
- Carballo M, Quiros RM. To treat or not to treat: the role of adjuvant radioiodine therapy in thyroid cancer patients. J Oncol 2012;2012:707156.
- Lee SL. Complications of radioactive iodine treatment of thyroid carcinoma. J Natl Compr Canc Netw 2010;8:1277-86. [PubMed]
- Lang BH, Lo CY, Wong IO, et al. Impact of second primary malignancy on outcomes of differentiated thyroid carcinoma. Surgery 2010;148:1191-6; discussion 1196-7. [PubMed]


