Technical hints and potential pitfalls in modified radical neck dissection for thyroid cancer
Introduction
Appropriate surgical management has become the mainstay treatment of differentiated thyroid cancer (1). Total thyroidectomy, central neck dissection and, when indicated, lateral neck dissection have now been implemented in most referral centers as the standard of surgical care whereas the use of radioiodine is whithering, largely because it rests on controversial evidence built in the 70’s and 80’s when inappropriate surgical was common worldwide (2). Despite the biased ATA guidelines still recommend routine RAI ablation and the repeated use of stimulated Tg values, in the real world, well-operated differentiated low risk thyroid cancers—which represent 75-85% of all thyroid cancers are being increasingly followed-up with low intensity protocols due to the high efficacy of appropriate surgery to prevent recurrence and in rendering patients thyroglobulin-negative.
With the increased awareness of the relevance of lateral neck nodal disease in papillary cancer, modified radical neck dissection (MRND) is now more often performed, either synchronously with thyroidectomy or metachronously if recurrence is detected during follow-up. In our unit, 30-40% of patients with papillary cancer >1 cm will eventually require a MRND. Lateral neck dissection is also well-established for the initial treatment of many, if not all, medullary thyroid carcinomas. MRND implies the careful skeletonization of many relevant anatomical structures and should only be performed by appropriately trained surgeons. This article deals with the most important steps of MRND and the pitfalls that the surgeon may face in each of them. Its purpose is not to describe in detail the surgical technique of MRND, but to warn the trainee and the less experienced surgeon dealing with this procedure about the origin and causes of technical complications and pitfalls during lymph node neck dissection.
The surgeon must be aware that nodal clearance for thyroid cancer should be comprehensive, thorough and compartment-oriented. There is no role for node picking or single compartment dissection. Recurrences after MRND range from 10% to 50% (3) and are usually linked to an incomplete initial surgical procedure, particularly in patients over 55 years of age with large (>3 cm) nodal metastasis (4). The most commonly performed lymph node dissection for thyroid cancer involves a selective approach with clearance of compartments IIa, III and IV (5,6). The most common variant is to enlarge the dissection field to compartments IIb and V in cases of massive lymphatic involvement. Resection of the sternocleidomastoid muscle (SCM) and the accessory nerve is only exceptionally performed in neck dissections for thyroid cancer, but the internal jugular vein (IJV) is often resected due to its infiltration by large nodal metastasis. Unilateral excision of the IJV does not carry additional morbidity nor neck deformities as happens with muscular or accessory nerve resections.
Surgical technique at our institution
Our technical approach to MRND (or functional neck dissection) follows the steps thoroughly described and illustrated by Gavilán et al. (7) of the Osvaldo Suárez School. This approach puts particular emphasis on the complete removal of the cervical lymphatic nodes by encasing them within the middle cervical fascia, and on the preservation of the SCM, the IJV and the accessory nerve. When combined with total thyroidectomy, we do first the lateral neck dissection, second the same side thyroid resection and third the contralateral thyroidectomy.
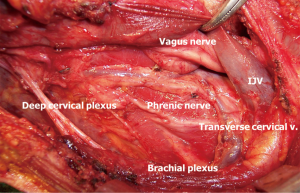
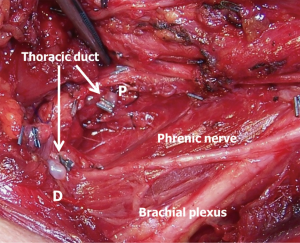
Briefly, a long transverse collar incision at the level of the cricoid cartilage is performed. J-shaped prolongation is rarely needed unless the patient has a long neck with massive involvement of compartments IIa and IIb. The SCM fascia is raised around the anterior and internal border of the muscle, the accessory nerve and the craneal end of the IJV are identified and a downwards dissection is performed to clear compartments IIa and III preserving the deep prevertebral fascia and as many branches as possible of the deep cervical plexus. Then the omohyoid muscle is cut or retracted and the dissection is carried out downwards preserving the transverse cervical vessels. The compartment IV is then cleared. At this stage, the more internal part of compartment V may be pulled from below the SCM and included in the specimen. The vagus nerve, the phrenic nerve and the brachial plexus are routinely identified and preserved. In the left side care is taken not to injure the thoracic duct. The specimen is then rotated medially, the carotid-middle cervical facia incised and the IJV unwrapped along its entire length.
The prevalence of postoperative hypocalcemia and permanent hypoparathyroidism are higher after total thyroidectomy and nodal dissection for thyroid cancer than after total thyroidectomy for benign conditions (8). For this reason, the surgeon must be particularly careful and skilled to adequately identify, dissect and preserve the parathyroid glands, particularly if a central neck dissection is also performed as we do routinely (9).
How to proceed?
The middle cervical fascia
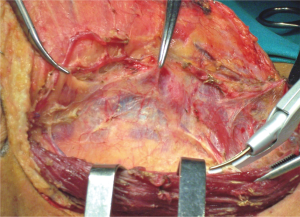
When performing the collar incision, care is taken not to cut through the SCM fascia. Once the skin flaps have been raised, the segment of the external jugular vein overlying the SCM is excised and the SCM fascia is elevated (Figure 1) to unwrap de SCM and enter the neck vascular space externally, through the middle fascial plane. The SCM fascia continues with the fascia enveloping the IJV and the carotid artery and is used as a reference landmark all over the procedure. The raised fascia will be used as an envelope containing all the lymphonodal tissue around the IJV. Failure to do so will hamper the complete removal of nodes in compartments IIa-IV. Some perforating vessels are dealt with during this step (Figure 1). When transecting the external jugular vein at the level of the posterior border of the SCM, care should be taken not to injure a branch that, occasionally, communicates this vein with the IJV running below the muscle. This can lead to troublesome bleeding coming from the IJV, still hidden by the SCM.
The spinal accessory nerve
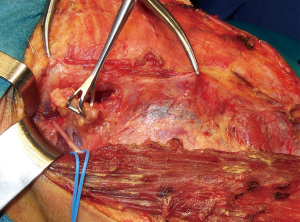
Once the SCM fascia has been dissected off the muscle from the mastoid to the clavicle over its inner and deeper surfaces, the accessory nerve is identified high in the surgical field. A low approach may miss the segment of the accessory nerve running between the SCM and the IJV (Figure 2) and the surgeon will encounter the deep cervical plexus, a thick branch of which may be mistaken for the accessory nerve. Careful use of cautery will stimulate the nerve (and produce a contraction of the trapezius muscle) prior to actually identifying it. Once identified, the accessory nerve is looped and dissected from the SCM internal border to the IJV which lies either anterior (30%) or posterior (70%) to the nerve (Figure 3). An anterior course of the IJV facilitates the unintentional damage to its lateral side during accessory nerve dissection. The IIa compartment is cleared and the floor of the surgical field is bluntly dissected without entering the deep cervical facia. A too deep dissection will mislead the surgeon into the splenius and levator scapulae muscles eventually transecting the phrenic nerve it its most superior course. If the compartment IIa is obviously involved, the IIb nodes—above and posterior to the accessory nerve—have to be dissected (10,11). This can be done by careful upwards lifting of the nerve and gentle pulling of the IIb nodes below the nerve (Figure 4). This is the only extrafascial lymph node group of the whole neck dissection.


The deep cervical fascia and the floor of MRND
Once compartment II has been cleared, the deep fascia appears exposed as the “floor” of the surgical field, just caudal and posterior to the accessory nerve. Staying superficial to the deep fascia along the whole procedure is crucial to avoid damaging the brachial plexus and the phrenic nerve. The dissection then proceeds downwards and the surgeon will now encounter the deep cervical plexus running over the deep fascia and below the SCM to innervate the skin around the shoulder and the high chest area (Figure 5). In most cases all or most of the branches of the cervical plexus can be preserved thus preventing or alleviating shoulder pain, a common sequel of MRND. Furthermore, some of the branches of the deep plexus anastomose with the accessory nerve contributing with some motor fibers. The dissection then proceeds downwards uncovering the levator scapulae muscle externally and the anterior and middle scalene muscles medially.
The transverse cervical vessels
The specimen is now rotated medially down to the crossing of the omohyoid muscle. The muscle can be preserved or cut according to the patient’s anatomy and the extension of the nodal involvement. At this stage the transverse cervical vessels are identified lying anterior to the deep fascia and are preferably left in situ. The distal transection of these vessels implies its inclusion in the specimen and that they should be ligated again close to the subclavian vessels. Injurying the transverse vessels at their origin may cause troublesome hemorrhage deep in the neck close to the midline. Leaving the transverse cervical vessels in situ provides a good landmark to preserve the deep fascia overlying the scalene muscles and the phrenic nerve. If these vessels are transected distally and lifted up with the specimen, the surgeon risks entering the plane below the deep fascia where the brachial plexus and the phrenic nerve may be injured (Figures 5,6). There are numerous variations of the branching of the transverse cervical vessels and the thyrocervical trunk that should make the surgeons cautious at this stage of the operation (7).

The proximal end of the jugular vein
Compartments III and IV are the most commonly involved in thyroid cancer. Thus, dissection around the proximal end of the IJV, close to its junction with the subclavian vein, becomes an important step in MRND. The surgeon must take care not leaving behind involved nodes that may hide dorsally to the IJV or that may extend laterally towards compartment V. At this point, medial traction of the specimen by the assistant to facilitate the dissection, results in the vein folding and becoming vulnerable to sharp dissection. Torsion of the proximal end of the IJV attenuates or completely blocks blood flow and the surgeon loses sight of the vein walls that may be then inadvertently punctured with the scalpel blade or the scissors.
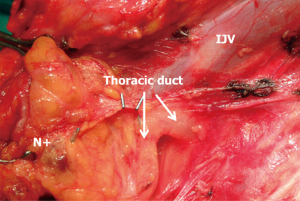
The thoracic duct
Large metastatic nodes in the left IV compartment pose a threat to the integrity of the thoracic duct since it usually lies deep close to the enlarged nodes. Extremely cautious dissection should be done around the distal segment of the left IJV, particularly when it joins the left subclavian vein. The thoracic duct is usually identified as a thin-walled conduct filled with whitish fluid (Figure 7). If it is injured, lymph usually flows out and is easily detected by the experienced surgeon. If the thoracic duct has been damaged, both ends should be identified and ligated or clipped (Figure 8). Failure to do so will lead to a chyle leak in the immediate postoperative period with its attendant morbidity (12). Independently of whether or not a major lymph duct injury has occurred, meticulous lymphostasis around the proxymal end of both IJVs is a must to prevent lymphatic fistulas and seromas. A Valsalva maneuver may help to identify lymphatic leakage.
The compartment V
Dissection of the supraclavicular fossa in thyroid cancer remains a controversial issue. The prevalence of node metastasis in this compartment varies from 15% to 50%. Level V lymphadenectomy may lead to spinal accessory nerve injury and increases shoulder pain. Most authors follow a selective approach to level V lymphadenectomy which may be only indicated in patients with lymph node metastasis in the ipsilateral lateral neck with macroscopic extranodal extension (13). In most cases, part of the level V compartment is excised in continuity with level IV dissection, by pulling the supraclavicular fibrofatty tissue from below the SCM.
If formal compartment V dissection is warranted, we usually start the MRND by clearing the supraclavicular fossa and by first identifying the accessory nerve deep to Erb’s point. Some branches of the deep cervical plexus follow a similar course than the accessory nerve and may mislead the novice surgeon. This is the most demanding part of compartment V dissection. The fibrofatty tissue of the supraclavicular fossa is then pulled downwards around the omohyoid muscle, preserving the most lateral segment of the transverse cervical vessels that can be identified overlying the fascia of the elevator scapula muscle (Figure 9). Dissection proceeds down to the subclavian vein and close to compartment IV. We then leave the compartment V specimen in situ and proceed to clear compartments II and III. Then, the compartment V specimen is pulled to the midline below the SCM and the compartment IV dissection is performed.

Conclusions
If properly done, MRND is not a too invasive surgical procedure and patients can be discharged from the hospital on the second to fourth postoperative day. For a smooth postoperative course, the following advices seem pertinent to avoid pitfalls during MRND for thyroid cancer and are a good summary of the text above:
- Start by appropriately elevating the SCM fascia;
- Do not miss the accessory nerve;
- Do not go deep below the deep cervical fascia;
- Preserve the deep cervical plexus;
- Preserve the transverse cervical vessels;
- Identify the brachial plexus, the phrenic nerve and the vagus nerve;
- Beware of IJV torsion when dissecting the compartment IV;
- Identify and clip all lymphatic leaks after dissecting left and/or right IV compartments;
- Dissect selectively compartments IIb and V according to cancer extension.
Acknowledgements
This manuscript has not been submitted elsewhere for publication.
Disclosure: The authors declare no conflict of interest.
References
- Grant CS, Stulak JM, Thompson GB, et al. Risks and adequacy of an optimized surgical approach to the primary surgical management of papillary thyroid carcinoma treated during 1999-2006. World J Surg 2010;34:1239-46. [PubMed]
- Hay ID. Selective use of radioactive iodine in the postoperative management of patients with papillary and follicular thyroid carcinoma. J Surg Oncol 2006;94:692-700. [PubMed]
- de Meer SG, Dauwan M, de Keizer B, et al. Not the number but the location of lymph nodes matters for recurrence rate and disease-free survival in patients with differentiated thyroid cancer. World J Surg 2012;36:1262-7. [PubMed]
- Ito Y, Kudo T, Takamura Y, et al. Lymph node recurrence in patients with N1b papillary thyroid carcinoma who underwent unilateral therapeutic modified radical neck dissection. World J Surg 2012;36:593-7. [PubMed]
- Caron NR, Tan YY, Ogilvie JB, et al. Selective modified radical neck dissection for papillary thyroid cancer-is level I, II and V dissection always necessary? World J Surg 2006;30:833-40. [PubMed]
- Lee J, Sung TY, Nam KH, et al. Is level IIb lymph node dissection always necessary in N1b papillary thyroid carcinoma patients? World J Surg 2008;32:716-21. [PubMed]
- Gavilán J, Herranza J, DeSanto LW, et al. Functional and selective neck dissection. New York: Thieme Medical Publishers, Inc. 2002.
- Sitges-Serra A, Ruiz S, Girvent M, et al. Outcome of protracted hypoparathyroidism after total thyroidectomy. Br J Surg 2010;97:1687-95. [PubMed]
- Pereira JA, Jimeno J, Miquel J, et al. Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery 2005;138:1095-100, discussion 1100-1. [PubMed]
- Lee BJ, Wang SG, Lee JC, et al. Level IIb lymph node metastasis in neck dissection for papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 2007;133:1028-30. [PubMed]
- Farrag T, Lin F, Brownlee N, et al. Is routine dissection of level II-B and V-A necessary in patients with papillary thyroid cancer undergoing lateral neck dissection for FNA-confirmed metastases in other levels. World J Surg 2009;33:1680-3. [PubMed]
- Nussenbaum B, Liu JH, Sinard RJ. Systematic management of chyle fistula: the Southwestern experience and review of the literature. Otolaryngol Head Neck Surg 2000;122:31-8. [PubMed]
- Shim MJ, Roh JL, Gong G, et al. Preoperative detection and predictors of level V lymph node metastasis in patients with papillary thyroid carcinoma. Br J Surg 2013;100:497-503. [PubMed]


